European Journal of Neurodegenerative Diseases 2023; 12(1):January-April 1-4
SIDE EFFECTS OF STATINS, INCLUDING NEUROLOGICAL DISORDERS: NEW ADVANCES
F. Carinci
Department of Translational Medicine, University of Ferrara, Ferrara, Italy
Correspondence to:
Prof. Francesco Carinci
Department of Translational Medicine,
University of Ferrara,
Ferrara, Italy
e-mail: crc@unife.it
ABSTRACT
Statins are drugs that, through blocking hydroxy-methylglutaryl coenzyme A reductase, can decrease low-density lipoprotein (LDL) and triglyceride blood levels. With apparent efficacy, these drugs protect blood vessels and reduce the risk of cardiovascular events and strokes. However, like other drugs, statins can cause side effects, such as muscle pain, diabetes, gastrointestinal disorders, dementia and cognitive diseases, even if there is contradictory evidence that statins by lowering cholesterol levels may be protective in the brain. Here, we report some side effects of statins and their impact on the central nervous system (CNS).
KEYWORDS: Statins, side effects, neurological, CNS
INTRODUCTION
Statins are a class of drugs that lower low-density lipoprotein (LDL) cholesterol in subjects with aortic, coronary, or carotid stenosis and protect against ischemic attacks, strokes, and cardiovascular events. These drugs have beneficial effects, reducing the frequency of heart attacks and lowering the frequency of mortality (1). Statins are hydroxy-methyl-glutaryl-coenzyme A (HMG-CoA) reductase inhibitors which the body tolerates very well. However, they cause side effects such as muscle symptoms, diabetes mellitus, and brain disorders. The risks of side effects due to these lipid-lowering drugs are less than the benefits of lowering cholesterol levels. Patients taking statins may present myalgia in 9-20% of cases and may develop, albeit rarely, autoimmune myopathy and rhabdomyolysis (2). In addition, antibodies to HMG-CoA reductase may be generated, which could cause the symptoms associated with statins. However, the diagnosis of statin side effects is complex, and if these effects do occur, switching treatment to other lipid-lowering drugs is advisable.
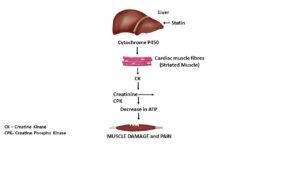
Rhabdomyolysis
Rhabdomyolysis can occur (with a frequency of less than 10%) or can be amplified in patients taking statins (3). It is a disease involving skeletal muscle tissue breakdown with symptoms of muscle weakness, myalgias, and reddish-brown urine. In this disease, there may be a nonspecific increase in creatine kinase (CK) levels with renal impairment, representing a diagnostic element. CK, also called creatine phosphokinase (CPK), is an enzyme produced by a striated muscle that catalyzes the reaction of creatinine into phosphocreatine with the consumption of ATP. CK is found in the bloodstream after muscular exertion or after taking statins (4). The increase in CK can occur after prolonged physical exercise in athletes who do not take statins. Elevated CK levels represent a sensitive laboratory index of muscle injury and often aid in diagnosing statin-associated symptoms. Therefore, the statin treatment of patients with high CK levels should always be considered. The appearance of rhabdomyolysis in subjects taking statins is very low and depends on the dose, advanced age, physical disability, a lower body mass index, and on the general physical condition of the patient (5). There is a correlation between dosage and symptoms; the higher the dose, the higher the frequency of statin-associated symptoms (2). Statins are mainly processed and catabolized in the liver by cytochrome P450 which transforms lipids into hydrophilic complexes that are subsequently eliminated (6) (Fig. 1).
|
Diabetes mellitus
Additionally, it has been reported that subjects treated with statins may develop diabetes mellitus with blood glucose values above 100 mg/dl (7); this appears to have a higher incidence in older women than in men. The mechanism of action of statins on diabetes mellitus is not yet clear, but it is known that low blood cholesterol levels are associated with an increased risk of diabetes (8); this is because cholesterol could affect the pancreatic production of insulin with an alteration of glucose metabolism, although the risk is low and exceeded by the beneficial effects of statins (9). Furthermore, in addition to the benefits of statin therapy, their preventive use could prevent vascular events, including myocardial infarction and stroke, and interrupting therapy could cause brain and heart damage (10).
Neurological complications
Statins can also cause undesirable effects on the brain system and, in particular, on cognition. It is known that increased fat in the bloodstream correlates to the onset of some neurological symptoms, including dementia (11). In some cases, statin treatments reduce the incidence of these brain diseases and therefore protect the brain (12). However, statins appear to reduce cognitive dysfunction risk, which could be important in degenerative diseases such as Alzheimer’s (13). Although there are not many studies on the effect of statins on the CNS, cholesterol inhibition could affect brain function, but this is quite unlikely since cholesterol has no active participation in the brain (14). In support of the thesis that statins protect the CNS, data shows that these cholesterol inhibitors can enhance neuron learning function, inhibit amyloid-beta, and reduce brain inflammation (15-17).
Furthermore, low cholesterol levels caused by statin treatment can cause a mild depressive syndrome, also related to the lowering of serotonin (18). However, all these CNS effects of statins still need to be confirmed. Furthermore, because statins can cause muscle problems, they could affect the myocardium, although there are currently no satisfactory scientific articles on the direct effect of these drugs on the myocardium (19). Therefore, it would be interesting to study the biological effects of statins on myocytes in vitro to improve their efficacy and possibly reduce the side effects, if any.
CONCLUSION
Here, in this short review, we can conclude that statins can increase CK, causing muscle pain, and may have effects on the brain that are not yet clear. However, it seems that they could be protective since the lowering of cholesterol leads to better cerebral blood circulation, resulting in the improvement of cognitive functions and the inhibition of inflammatory parameters (20).
Conflict of interest
The author declares that they have no conflict of interest.
REFERENCES
- Paraskevas KI, Gloviczki P, Antignani PL, et al. Benefits and drawbacks of statins and non-statin lipid lowering agents in carotid artery disease. Progress in Cardiovascular Diseases. 2022;73:41-47. doi:https://doi.org/10.1016/j.pcad.2022.05.003
- Mammen AL, Amato AA. Statin myopathy: a review of recent progress. Current Opinion in Rheumatology. 2010;22(6):644-650. doi:https://doi.org/10.1097/bor.0b013e32833f0fc7
- Mendes P, Robles PG, Mathur S. Statin-Induced Rhabdomyolysis: A Comprehensive Review of Case Reports. Physiotherapy Canada. 2014;66(2):124-132. doi:https://doi.org/10.3138/ptc.2012-65
- Torres PA, Helmstetter JA, Kaye AM, Kaye AD. Rhabdomyolysis: pathogenesis, diagnosis, and treatment. The Ochsner journal. 2015;15(1):58-69.
- Safitri N, Alaina MF, Pitaloka DAE, Abdulah R. A Narrative Review of Statin-Induced Rhabdomyolysis: Molecular Mechanism, Risk Factors, and Management. Drug, Healthcare and Patient Safety. 2021;Volume 13:211-219. doi:https://doi.org/10.2147/dhps.s333738
- Thompson PD, Panza G, Zaleski A, Taylor B. Statin-Associated Side Effects. Journal of the American College of Cardiology. 2016;67(20):2395-2410. doi:https://doi.org/10.1016/j.jacc.2016.02.071
- Raghuvir Keni, Sekhar A, Karthik Gourishetti, et al. Role of Statins in New-onset Diabetes Mellitus: The Underlying Cause, Mechanisms Involved, and Strategies to Combat. Current Drug Targets. 2021;22(10):1121-1128. doi:https://doi.org/10.2174/1389450122666210120125945
- Chogtu B. Statin use and risk of diabetes mellitus. World Journal of Diabetes. 2015;6(2):352. doi:https://doi.org/10.4239/wjd.v6.i2.352
- Galicia-Garcia U, Jebari S, Larrea-Sebal A, et al. Statin Treatment-Induced Development of Type 2 Diabetes: From Clinical Evidence to Mechanistic Insights. International Journal of Molecular Sciences. 2020;21(13):4725. doi:https://doi.org/10.3390/ijms21134725
- Konstantinos Tziomalos, Athyros VG, Mikhailidis DP. Statin discontinuation: an underestimated risk? Current Medical Research and Opinion. 2008;24(11):3059-3062. doi:https://doi.org/10.1185/03007990802469102
- Morris MC, Tangney CC. Dietary fat composition and dementia risk. Neurobiology of Aging. 2014;35:S59-S64. doi:https://doi.org/10.1016/j.neurobiolaging.2014.03.038
- Schultz BG, Patten DK, Berlau DJ. The role of statins in both cognitive impairment and protection against dementia: a tale of two mechanisms. Translational neurodegeneration. 2018;7:5. doi:https://doi.org/10.1186/s40035-018-0110-3
- Chu CS, Tseng PT, Stubbs B, et al. Use of statins and the risk of dementia and mild cognitive impairment: A systematic review and meta-analysis. Scientific Reports. 2018;8(1). doi:https://doi.org/10.1038/s41598-018-24248-8
- Kosowski M, Smolarczyk-Kosowska J, Marcin Hachuła, et al. The Effects of Statins on Neurotransmission and Their Neuroprotective Role in Neurological and Psychiatric Disorders. Molecules. 2021;26(10):2838-2838. doi:https://doi.org/10.3390/molecules26102838
- Schreurs BG. The effects of cholesterol on learning and memory. Neuroscience & Biobehavioral Reviews. 2010;34(8):1366-1379. doi:https://doi.org/10.1016/j.neubiorev.2010.04.010
- Rudajev V, Novotny J. Cholesterol as a key player in amyloid β-mediated toxicity in Alzheimer’s disease. Frontiers in Molecular Neuroscience. 2022;15. doi:https://doi.org/10.3389/fnmol.2022.937056
- Chen Y, Yin M, Cao X, Hu G, Xiao M. Pro- and Anti-inflammatory Effects of High Cholesterol Diet on Aged Brain. Aging and Disease. 2018;9(3):374-390. doi:https://doi.org/10.14336/AD.2017.0706
- Sun S, Yang S, Mao Y, Jia X, Zhang Z. Reduced cholesterol is associated with the depressive-like behavior in rats through modulation of the brain 5-HT1A receptor. Lipids in Health and Disease. 2015;14(1). doi:https://doi.org/10.1186/s12944-015-0020-7
- Mollazadeh H, Tavana E, Fanni G, et al. Effects of statins on mitochondrial pathways. Journal of Cachexia, Sarcopenia and Muscle. Published online January 29, 2021. doi:https://doi.org/10.1002/jcsm.12654
- Duan Y, Gong K, Xu S, Zhang F, Meng X, Han J. Regulation of cholesterol homeostasis in health and diseases: from mechanisms to targeted therapeutics. Signal Transduction and Targeted Therapy. 2022;7(1):1-29. doi:https://doi.org/10.1038/s41392-022-01125-5